Pregnancy in Adolescents
Pregnancy in Adolescents
Magnitude of problems related to adolescent pregnancy
- 47% of Indian women are married before they attain 18 years of age (NFHS 3)
- TFR amongst 15-19 years is 14% in urban & 18% in rural of the total fertility (NFHS 3)
- Unmet need of family planning in the 15-19 years age group is 27% (NFHS 3)
- 20% of the pregnant girls below 20 years of age have not had antenatal checkup
- 66.2% of the pregnant girls below 20 years of age have received iron & folate tablets as part of antenatal care
- For a mother <20 of age, 34% of birth where assisted by doctors, 13% by ANMs and 36% by TBAs.
- More than 60% of mothers below 20 years of age had not received post partum checkup
- Maternal mortality due to teenage pregnancy is 9% (2007-2009)
- Still birth, early neonatal deaths and infant mortality is higher in girls aged <20 years.
- Infant mortality and incidence of low birth weight babies is higher in adolescent mother.
Factors influencing adolescent pregnancy and childbirth
A range of social, cultural, biological and service delivery factors contribute to the high levels of adolescent pregnancy and childbirth:
- Declining age of menarche - The age of menarche (onset of first menstruation) has declined, especially in urban areas.
- Duration of education and societal demands - A growing number of adolescent girls are allowed to go for higher education and marry late as a result. But in rural areas, marriage still appears very early for young girls. They are then pushed into early motherhood.
- Early initiation of sexual activity is on the increase.
- Sexual coercion and rape, figures prominently in the lower socio-economic strata. Pregnancies are not the only result, but also serious physical and psychological consequences.
- Disruption of education also influences adolescent childbearing as women with little or no education are more likely to become mothers early.
- Socio-economic factors often force young girls into sexual exploitation and prostitution and compounded by lack of access to contraceptive services and inability to negotiate condom use, the young girl may soon become pregnant.
- Lack of access to information has a significant bearing on early pregnancy and childbirth.
- Lack of access to services leads to risky pregnancy and unsafe abortion,etc.
- Adolescent pregnancies tend to be highest in areas with the lowest contraceptive prevalence. Contraceptive prevalence has increased mostly among older, married women and not adolescents.
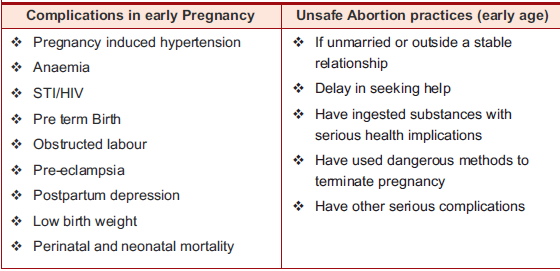
Complications in adolescent pregnancy and childbirth
Pregnancy and childbirth in adolescence are risky for the health of both mother and baby
- Biologically, an adolescent’s body is still developing and not yet ready to take on an added strain. The pelvic bones are not fully mature, and cephalo- pelvic disproportion could occur. Her body has special nutritional needs and when pregnancy occurs, it is a strain on already depleted reserves, especially if she belongs to a low socio-economic background. The young girl may not be mentally prepared for motherhood with all its added responsibilities, etc. and this could give rise to mental health problems like depression.
- Socio-culturally, pregnancy outside of marriage bears a terrible stigma and the above situation worsens when the girl is not married, in which case she does not get the emotional support she needs as well as support in terms of nutrition, rest, antenatal check-ups, etc.
This situation is not unique to unmarried adolescents as the married ones may not be aware of the importance of antenatal care. For various reasons, the adolescent woman is more likely to deliver at home. The older women in the home feel that a traditional birth attendant is equipped to carry out the delivery, her services are cheaper and she is easily accessible. A trained birth attendant or a hospital is usually thought of when things get out of hand and complications have already set in.
The risks are high, starting from the antenatal period, through labour and the postpartum period. Adolescent mothers are most likely to give birth to low weight babies and both the mother and child face higher mortality and morbidity.
Pregnancy related complications that occur more commonly in adolescents than in adults
- Death
- Pregnancy-induced hypertension
- Anaemia during antenatal period
- STIs/HIV
- Higher severity of malaria
- Pre-term birth
- Obstructed labour
- Anaemia during postpartum period
- Pre-eclampsia
- Postpartum depression
- Too early repeat pregnancies
- Low birth weight
- Perinatal and neonatal mortality
- Inadequate child care and breastfeeding practices
Problems in the antenatal period
- Pregnancy-induced hypertension: Studies report an increased incidence of the condition in young adolescents, when compared with women aged 30-34 years.
- Anaemia: There is an increased risk of anaemia in adolescents because of nutritional deficiencies, especially of iron and folic acid, and by malaria and intestinal parasites.
- STIs/HIV: Sexually active adolescents are at an increased risk of contracting STIs, including HIV infection, owing to their biological and social vulnerability. There is also the increased risk of mother-to child transmission of HIV in adolescents, because the HIV infection is more likely to be recent, and therefore associated with higher viral loads. The presence of other STIs (syphilis, gonorrhoea and chlamydia) with local inflammation may increase viral shedding, thereby increasing the risk of transmission during labour.
- Higher severity of malaria is often seen in first time pregnant women (which includes many adolescents) and is a common cause of anaemia in this group. This puts them at risk and their unborn babies at risk of intra-uterine death.
Problems during labour and delivery
- Pre-term birth is common in women under twenty years of age because of immaturity of the reproductive organs, social factors such as poverty, at play.
- Obstructed labour in young girls (below 15 years of age) occurs due to the small size of the birth canal leading to cephalo-pelvic disproportion. Lack of access to medical and surgical care can result in complications like vesicovaginal and recto-vaginal fistulae.
Problems in the postpartum period
- Anaemia is commoner and further aggravated by blood loss during delivery thereby also increasing the risk of infection.
- Pre-eclampsia: Several studies report that pre-eclampsia occurs more often in young adolescents. The symptoms may worsen and sometimes recognized only during the first postpartum days.
- Postpartum depression and common mental health problems are common due to reasons described above.
- Too early repeat pregnancies, especially in unmarried adolescents can occur because of the difficulty in accessing reliable contraception.
Problems affecting the baby
- Low birth weight: There is a higher incidence of low birth weight (weight <2500 grams) among infants of adolescent mothers.
- Perinatal and neonatal mortality is increased in infants of adolescent mothers, compared with infants of older mothers.
- Inadequate childcare and breastfeeding practices: Young mothers, especially those who are single and poor, may find it hard to provide their children with the adequate care. This is reflected in their poor child feeding, including breastfeeding, practices.
Care of adolescents during pregnancy, childbirth and postnatal period
Adolescent pregnancies and deliveries require much more care than adult pregnancies and all efforts must be made to reduce the occurrence of problems. This includes early diagnosis of pregnancy, effective antenatal care, effective care during labour and delivery, and during the postpartum period.
Pre-pregnancy Counselling
- Contraceptive counselling
- Building up haemoglobin
- Folic acid supplementation
- Detection and treatment of pre-existing medical diseases
- Thalassemia screening
- Rubella vaccination.
Early diagnosis of pregnancy
Health service providers and other adults like family members in more regular contact with the adolescent, have the shared responsibility of creating an environment in which she feels able to share information about her situation, especially if she is unmarried. She may not know that she is pregnant because she may not remember the dates of her last menstrual period, or because her periods are not regular. She may even want to hide her pregnancy or seek ways of terminating it. Being aware of these issues, and being on the lookout for telltale signs of early pregnancy such as nausea will help ensure an early diagnosis of pregnancy so that care is started early and complications are avoided.
Antenatal care
Many complications can be detected and many can be avoided if the adolescent is able to access good antenatal services. Pregnancy-induced hypertension (Pre-eclampsia) can easily be detected and referred to the PHC for management. In case of more serious complications (such as pre-eclampsia, eclampsia, and abruptio placentae), referral to a woman’s hospital is essential. Anaemia and malaria too can be detected and treated during routine antenatal care. Screening for STIs can lead to early referral and early treatment, if required. Iron and folic acid supplements will prevent anaemia to a large extent. Most importantly, antenatal visits could help identify those adolescents, who are at risk of preterm labour, though interventions to address this are limited.
Antenatal care also provides a valuable opportunity for the provision of information and counseling support that adolescents need. This is especially important in the case of adolescents, especially unmarried ones, because of their greater need for support.
Counseling during pregnancy
Information and counseling support is the right of every pregnant woman who reaches a health centre and pregnant adolescents have special needs and questions and concerns of their own. They must be given an opportunity to raise and discuss these issues.
Their needs must be matched with competent and sensitive counseling support in terms of the socio-cultural environment that has to be faced, the options available in terms of the pregnancy; the access to health services for routine antenatal care and in case of emergency; the danger signs that need to be aware of, etc.
Counseling should also include care of the newborn and prevention of an early repeat pregnancy.
Since adolescents are more at risk of STIs including HIV/AIDS, voluntary counseling and testing (VCT) services should be made available to them. As ANMs/LHVs, you should know where the nearest VCT centres is, to be able to refer your clients for screening.
Management of labour and delivery
If the pregnancy in an adolescent is normal and with no complications and anaemia is treated adequately, labour starts at term, and the infant is in cephalic presentation, labour is not at increased risk. Counsel the client for institutional delivery at PHC.
However, if the adolescent is severely anaemic, postpartum haemorrhage can be a dangerous possibilty. In very young adolescents, pre-term labour as well as obstructed labour are more likely to occur. Such adolescents are at high risk and it is advisable to encourage hospital delivery. The family should be advised to make arrangements for transportation to the hospital, when needed.
Besides observing and monitoring, supporting the woman is very important and studies have shown that continuous empathetic support during labour, provided by a technically qualified nurse or midwife results in many benefits both to the mother and the baby.
Postpartum care
This includes the prevention, early diagnosis and treatment of postnatal complications in the mother and her baby. It also includes information and counselling on breastfeeding, nutrition, contraception and care of the baby. The adolescent mother will require special support on how to care for herself and her baby.
Contraception: It is very important that too early repeat and unplanned pregnancies should not occur for lack of access to contraceptive services. The postpartum period presents a good opportunity for taking steps towards pregnancy prevention and for promoting dual protection by encouraging condom use.
Nutrition of the mother: The lactating adolescent needs adequate nutrition to meet her own as well as the extra needs required for breast-milk production.
Breastfeeding: Exclusive breast feeding is recommended for 6 months. A young adolescent, especially one who is single - would require extra support in achieving breastfeeding successfully.
Abortion
Adolescent pregnancy very often leads to unsafe abortion especially if the girl is unmarried. The consequences of this type of abortion can be life threatening. Although abortion is legal in India, it is estimated that four million Indian women a year still resort to illegal abortions because of social stigma, lack of awareness and lack of access to health facilities that offer technically competent services.
Medical Termination of Pregnancy Act
The Medical Termination of Pregnancy Act was passed in 1971. The Act was intended to grant women freedom from unwanted pregnancies, especially when there was social censure or medical risk involved. Apart from these benefits, it also ensured that abortion services became easily accessible.
The aim of the Act is to allow for the termination of certain pregnancies by registered medical practitioners. If a pregnancy is terminated by someone who is not a registered medical practitioner, it would constitute an offence punishable under the Indian Penal Code.
When MTP is permitted
According to the Act, abortion may be permitted only in certain cases:
- Where the length of the pregnancy does not exceed twelve weeks or
- Where the length of the pregnancy exceeds twelve weeks but does not exceed twenty weeks, if not less than two registered medical practitioners are, of opinion, formed in good faith, that, -
- the continued pregnancy would pose a risk of injury to the woman’s physical or mental health; or
- there exists a substantial risk that the foetus would suffer from a severe physical or mental abnormality; or
- the pregnancy resulted from rape or incest; or
- the continued pregnancy would significantly affect the social or economic circumstances of the woman; or
- After the 20th week of the gestation period if a medical practitioner, after consultation with another medical practitioner or a registered midwife who has completed the prescribed training course, is of the opinion that the continued pregnancy—
- Would endanger the woman’s life;
- Would result in a severe malformation of the foetus; or
- Would pose a risk of injury to the foetus.
As long as the above conditions are fulfilled, a doctor can terminate a pregnancy without fear of being prosecuted under the Indian Penal Code.
Whose consent is required?A pregnancy can be terminated only with the informed consent of the pregnant woman; no other person’s consent needs to be obtained.
In the case of a pregnant woman, less than eighteen years old, and in the case of a pregnant woman, more than eighteen years old but of unsound mind, the consent of her guardian must be obtained in writing.
Where can a MTP be performed?
MTPs can be performed only at the centres certified by the government. These centers could be located in public or private sector.
The rights of the pregnant woman
Whenever a woman requests that her pregnancy be terminated, she must be informed of her rights under the Act.
Also, whenever a pregnancy has been terminated, the medical practitioner should record the prescribed information. However, the name and address of the woman, who has requested or obtained a termination of pregnancy, should be kept confidential, unless she herself chooses to disclose that information.
Penalisation
If a person who is not a medical practitioner, who has not completed the prescribed training course, performs the termination of a pregnancy, can be convicted and penalised with a fine or imprisonment for a period not exceeding 10 years.
Sources :Last Modified : 2/12/2020
