Malnutrition in children
Malnutrition in children
Nutrition is acknowledged as one of the most effective entry points for physical and intellectual growth and development. It is a key Sustainable Development Goal. Optimum and appropriate nutrition is essential for women and children to survie, thrive and break the intergenerational cycle of malnutrition and poor health in the community.
Malnutrition
Malnutrition is one of the most important challenges facing contemporary India. While malnutrition is widely used to describe under nutrition, it actually represents both under and over nutrition. While under-nutrition results from inadequate consumption, poor absorption or excessive loss of nutrients, over-nutrition results from excessive energy and fat intake.
Under-nutrition and the Nutrition Gap
Under-nutrition is caused by several determinants such as low family income, large family size, gender bias, changing crop patterns due to various reasons leading to dietary imbalance, access to food, loss of traditional food habits, lack of knowledge etc. Poor health conditions such as diarrhoea and anaemia have a cascading effect which perpetuates under-nutrition.
Forms of Childhood Undernutrition
Under nutrition in children below five years of age in populations is measured by three anthropometric indices which are based on a comparison of the measured height and weight of the child compared to the WHO defined reference height and weight of children of the same age and sex. These three indices, viz., (i) weight-for-age, (ii) height/ length-for- age, (iii) weight- for-height/ length are used to identify underweight, stunting and wasting, respectively.
Underweight:
Underweight can result from either chronic or acute malnutrition or both. An underweight child has a weight-for-age Z-score at least two standard deviations below the median (-2 SD) for the World Health Organization (WHO) Child Growth Standards.
- Moderate Underweight (MUW) is defined as weight-for-age between -2 and -3 SD as per WHO growth standard.
- Severe Underweight (SUW) weight is a condition in which a child has a very low weight in relation to age (Z score of < - 3 SD), as per WHO child growth standards
- Stunting: Failure to achieve expected height/length as compared to healthy, well- nourished children of the same age is a sign of stunting. Stunting is an indicator of linear growth retardation. It is an indicator of chronic growth failure associated with a number of long-term factors including chronic insufficient nutrient intake, frequent infection and inappropriate feeding practices. A stunted child has a height-for-age Z-score that is at least two standard deviations (-2 SD) below the median for the WHO Child Growth Standards.
- Wasting: Wasting indicates current or acute malnutrition resulting from failure to gain weight or actual weight loss. Suboptimal Infant and Young child care and feeding practices including inadequate complementary feeding in older infants and young children from 6 months to 2 years of age, repeated enteric and respiratory tract infections are some of the factors leading to Severe Acute Malnutrition (SAM) in children. Wasting in individual children and population groups can change rapidly and shows marked seasonal variations associated with changes in food availability or disease prevalence to which it is very sensitive. A wasted child has a weight- for-height Z-score at least two standard deviations (-2 SD) below the median for the WHO Child Growth Standards.
- Moderate Acute Malnutrition (MAM) defined as weight-for-height between -2 and -3 SD as per WHO growth standard.
- Severe Acute Malnutrition (SAM) is a condition in which a child has a very low weight in relation to length/height (Z score of < - 3 SD), as per WHO child growth standards. SAM is a severe form of wasting.
Growth Faltering means growth rate below the standard for a child’s age & gender. It may include both weight and length/height are lower than standard.
Implications of Undernutrition
Undernutrition has an adverse impact on all stages of the life cycle, but some of the most damaging effects occur from conception to 1000 days of age. Prevention is important at this time. Besides contributing significantly to child mortality, irreversible brain damage can occur in this period of life. Both underweight and stunting set in early, in the first 2 years, when the child needs to be fed adequately and appropriately and is also exposed to frequent episodes of infections, particularly diarrhea. In India, the highest burden of under nutrition occurs between birth and two years of age; therefore, preventive measures need to predominantly address children under 2 years. Moreover, prevention of under nutrition during this period is important and requires initiatives to ensure that children are born healthy and with adequate weight. Once children settle into a growth curve at the end of 2 years, it is particularly difficult to shift the linear growth pattern upward, and recover from stunting. Indeed, attempts to overfeed such children entail a risk of them becoming overweight with higher propensity to develop non-communicable diseases as adults, including diabetes, hypertension and cardiovascular disease.
Therefore, it is critical to prevent under-nutrition, as early as possible, across the lifecycle, to avert irreversible cumulative growth and development deficits that impact maternal and child survival and health. It undermines the achievement of optimal learning outcomes during elementary education, impairs adult productivity and undermines gender equality.
Government Strategies to tackle undernutrition among children
The Government has taken several initiatives to break the intergenerational cycle of malnutrition. Adopting a life-cycle approach, interventions have been designed to meet the nutritional requirements of adolescent girls, pregnant women, lactating mothers and children through several schemes like POSHAN Abhiyaan, Anganwadi Services, Scheme for Adolescent Girls and Pradhan Mantri Matru Vandana Yojana (PMMVY) as direct targeted interventions to address the problem of malnutrition in the country.
POSHAN Abhiyaan
POSHAN Abhiyaan was launched on 8 March 2018, with an aim to achieve improvement in nutritional status of Adolescent Girls, Pregnant Women and Lactating Mothers in a time bound manner by adopting a synergised and result oriented approach. Further, the efforts under the Supplementary Nutrition Programme under Anganwadi Services and POSHAN Abhiyaan were rejuvenated and converged as ‘Saksham Anganwadi and POSHAN 2.0’ (Mission Poshan 2.0) to address the challenges of malnutrition in children, adolescent girls, pregnant women and lactating mothers through a strategic shift in nutrition content and delivery and by creation of a convergent ecosystem to develop and promote practices that nurture health, wellness and immunity.
Poshan 2.0 focuses on Maternal Nutrition, Infant and Young Child Feeding Norms, Treatment of MAM/SAM and Wellness through AYUSH. It rests on the pillars of Convergence, Governance, and Capacity-building. POSHAN Abhiyaan is the key pillar for Outreach and will cover innovations related to nutritional support, ICT interventions, Media Advocacy and Research, Community Outreach and Jan Andolan.
Under Poshan 2.0, focus is on diet diversity, food fortification, leveraging traditional systems of knowledge and popularizing use of millets. Nutrition awareness strategies under Poshan 2.0 aim to develop sustainable health and well-being through regional meal plans to bridge dietary gaps. Further, greater emphasis is being given on the use of millets for preparation of Hot Cooked Meal and Take Home rations (not raw ration) at Anganwadi centres for Pregnant Women, Lactating Mothers and Children below 6 years of age, as millets have high nutrient content which includes protein, essential fatty acid, dietary fibre, B-Vitamins, minerals such as calcium, iron, zinc, folic acid and other micro-nutrients thus helping to tackle anaemia and other micro-nutrient deficiencies in women and children. As per the Scheme Guidelines issued for Mission Saksham Anganwadi & Poshan 2.0, millets need to be mandatorily supplied at least once a week and suitably integrated in Take Home Ration (not raw ration) and Hot Cooked Meal in a palatable form.
Another key plank of the Abhiyaan are the Poshan Vatikas or Nutri-gardens that are being set up across the country to provide easy and affordable access to fruits, vegetables, medicinal plants and herbs.
Framework and Specific Details of Supplementary Nutrition
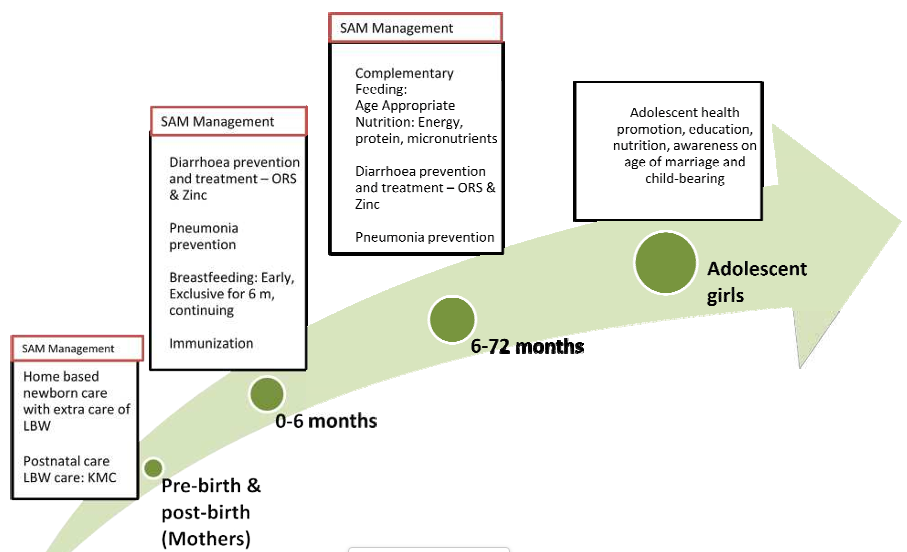
The services provided recognize that there is an intergenerational cycle of under nutrition, needing a comprehensive health and wellness approach, covering the entire life cycle of growth, with a focus on critical periods of nutritional vulnerability and opportunity for enhancing human development potential. The comprehensive health and wellness approach includes the following:
- Support for adolescent girls including their nutrition and skilling.
- Pre-birth nutrition support to pregnant women and post-birth to lactating mothers.
- Promotion of early initiation of breastfeeding and exclusive breast feeding in 0-6 month old infants.
- Promotion of age-appropriate and adequate complementary feeding starting from 6 months of age along with continued breastfeeding for 2 years or beyond.
- Ensuring dietary adequacy in children between 6 to 72 months.
- Prevention and management of early childhood illnesses
Comprehensive health and wellness approach towards life cycle of growth
Last Modified : 12/1/2023
This topic provides information about Poshan Abhiy...
This topic provides information about Health Wedne...
This topic provides information about ICDS and its...
This topic provides information about the Nigrani ...
